What is Diabetic Retinopathy?
Diabetic retinopathy (DR) is the most common cause of blindness in patients between 24 and 70 years old. Approximately half of all diabetics will develop diabetic retinopathy.
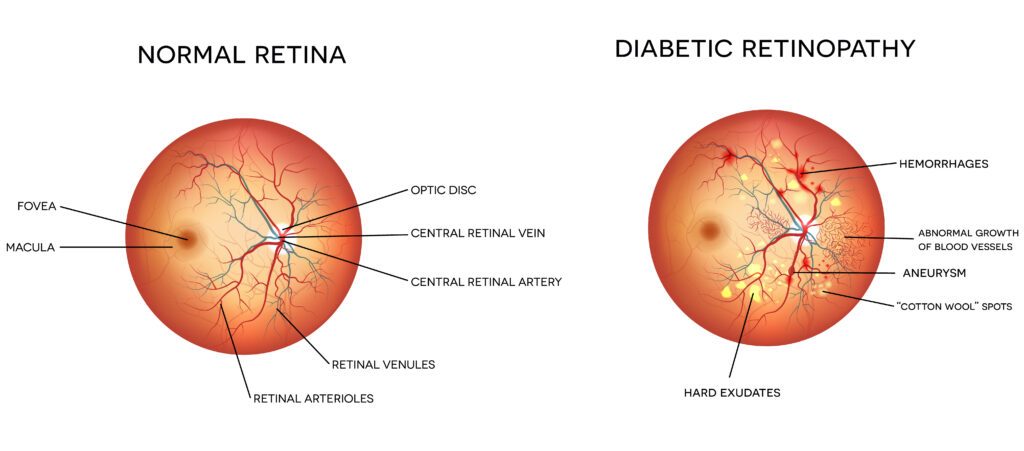
Diabetes mellitus (DM) affects not only the blood sugar level but also causes damage to small blood vessels throughout the body, including the eye. In diabetic retinopathy, high blood sugar levels cause damage to blood vessels in the retina which can impact vision. Because a person with early diabetes may have no symptoms, one may have had the eye condition for several years before it is diagnosed.
There are four main ways that diabetic retinopathy causes vision loss:
- Diabetic macular edema (DME): Fluid build up in the central portion of the retina
- Proliferative diabetic retinopathy (PDR): Growth of abnormal blood vessels into and on top of the retina
- Ischemia: retinal cell death or dysfunction due to lack of oxygen in the retinal tissue
- Bleeding: Bleeding can occur within the vitreous gel of the eye causing impaired vision
If you are diabetic, the American Academy of Ophthalmology recommends that you have your eyes dilated and the retina examined at least annually. The board-certified retina specialists at Georgia Retina are trained to diagnose diabetic retinopathy and help patients manage their condition. Early detection of diabetic retinopathy allows the best chance for maintaining good vision.
Types and Stages of Diabetic Retinopathy
Non-Proliferative Diabetic Retinopathy (NPDR)
NPDR is an early stage of diabetic retinopathy. Blood vessel damage can lead to abnormal leakage of fluid and blood into the retina. This may make the retina wet and swollen, a condition known as “edema.” If the center of the retina is affected, the condition is known as diabetic macular edema. This is the most common cause of visual loss in patients with diabetes and ranges from mild to severe.
Proliferative Diabetic Retinopathy (PDR)
PDR occurs when abnormal blood vessels grow into and on top of the retina. These blood vessels are weak and can break and bleed, causing vitreous hemorrhage. This can cause dark floaters and may cause immediate and severe loss of vision. If the bleeding is more severe, the entire inside of the eyeball can be filled with blood, partially or totally blocking vision. Pulling and contraction of these abnormal blood vessels and their associated scar tissue on the retina can lead to a traction retinal detachment, a condition where the retina is pulled away from the back of the eye leading to loss of vision.
Diagnosis
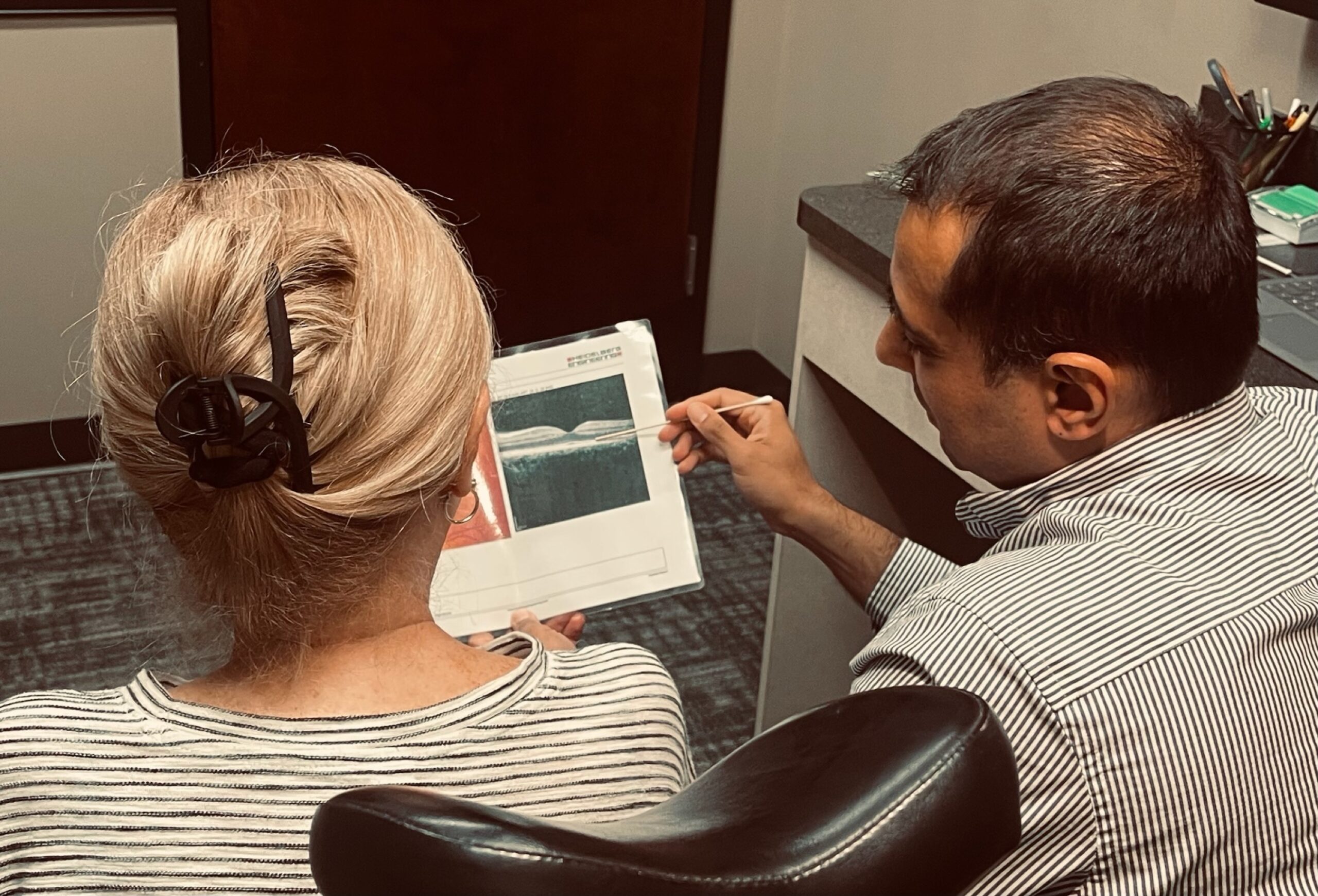
Diabetic retinopathy is diagnosed by your ophthalmologist during a dilated eye exam. Your doctor may obtain photographs of the retina and diagnostic tests, including ocular coherence tomography (OCT) and fluorescein angiography (FA), to help guide treatment. With OCT, light waves are used to capture detailed images of the retina. With FA, a special dye is injected into your bloodstream through an IV. This highlights the blood vessels in the retina so we can determine if there is any bleeding, leakage, or damage.
Treating Diabetic Retinopathy
Medical Treatment
Medical treatment for diabetic retinopathy may involve the use of injections of medicine into your eye (intravitreal injections) to treat buildup of fluid (diabetic macular edema). Recent science has shown that DME and PDR are controlled by a signal sent from damaged retina called vascular endothelial growth factor (VEGF). Several VEGF blocking drugs (Avastin, Lucentis, Eylea, Vabysmo) and other medications (steroids and steroid implants) when injected into the eye can cause DME and PDR to regress. Most of these agents provide only temporary relief and need to be given repeatedly over a prolonged period of time.
Surgical Treatments
If there is severe hemorrhage into the vitreous (the clear gel that fills the central cavity of the eye), surgery can be done to remove the vitreous jelly and the blood. This is known as vitrectomy surgery. This type of surgery may also be required if the abnormal blood vessels in the back of the eye form scar tissue, which pulls on the retina. This scar tissue may pull hard enough to lift the retina off the back of the eye like a tent. This situation is called a tractional retinal detachment.
Most vitrectomy surgeries are performed as outpatient procedures with local anesthesia, and the patient may go home the same day. Your surgeon will use a microscope and tiny instruments that are placed into your eye through small incisions in the sclera, the white part of the eye.
Laser Treatment
Macular edema can often be helped with a treatment known as focal laser treatment to attempt to seal off points where leaking is occurring. Laser eye surgery is a non-invasive treatment done in the office in which there are no incisions or cutting and no stitches. Numbing eye drops are used to ensure comfort during the procedure. This treatment results in an improvement in vision about 20-25% of the time.
The proliferative form of the disease is treated with a different kind of laser eye surgery known as panretinal photocoagulation (PRP). This treatment involves a greater number of applications and is sometimes done in two or three separate sessions. The peripheral portion of the retina is treated, which can cause side effects such as constriction of the visual field, as well as reduction in night vision. These side effects are relatively uncommon, and when they occur, are necessary tradeoffs to attempt to preserve the central vision.
Prognosis
Prevention is the best treatment for diabetic retinopathy. Optimal blood sugar, blood pressure, cholesterol and weight control can reduce the long-term risk of vision loss from diabetic retinopathy. Cooperation with your primary care physician is very important to help keep your diabetes and other cardiovascular risk factors under control. If you have any questions or concerns about diabetes management/treatment, please discuss them with your diabetic retinopathy specialist at Georgia Retina.